Do you often find yourself struggling with abdominal pain, cramping, and bloating that rarely seem to ease?
If so, you may be one of the many Canadians who struggle with irritable bowel syndrome.
Irritable Bowel Syndrome, or IBS for short, is one of the most common digestive issues in Canada, affecting 18% of people, according to the Canadian Digestive Health Foundation.
IBS affects the gut microbiome, which plays a crucial role in both digestion and nutrient absorption, your immune system, and even mental wellness. This means IBS can have a far-reaching impact beyond just stomach pain.
Let’s explore how taking control of your gut health can help you manage IBS symptoms, improve digestion, and support your overall well-being.
What is The Gut Microbiome?
Before we get into the specifics of IBS, it’s important to understand one of the main elements involved: the gut microbiome.
The gut microbiome refers to the trillions of microorganisms and bacteria that live in your digestive tract.
These microbes perform essential tasks, including breaking down complex foods, producing vital nutrients, and defending against harmful pathogens.
In fact, according to the Canadian Digestive Health Foundation, over 70% of your immune system resides in the gut, regulated in part by the diversity and health of your microbiome.
A balanced microbiome promotes harmony throughout your body, while an imbalance can lead to disruptions in both physical and mental health.
This makes maintaining a healthy microbiome key, and that’s where nutrition, lifestyle, and medical support come into play (we’ll touch on this more in later sections).
Signs You May Have Gut Microbiome Imbalance
You don’t need a microscope to know when your gut health is off. Symptoms of an imbalanced microbiome often appear across multiple body systems and may include:
- Persistent fatigue that doesn’t improve with rest
- Bloating or gas, especially after meals
- Mental fog or difficulty concentrating
- Disrupted sleep or trouble falling asleep
- Irregular bowel movements, including constipation or diarrhea
While these symptoms can stem from various causes, they’re also hallmark signs of a digestive imbalance.

IBS Basics – Symptoms, Types, and Causes
Living with IBS means dealing with more than the occasional upset stomach. For many, it’s a persistent condition that impacts daily comfort, mood, and quality of life.
Understanding the types of IBS and how it’s diagnosed is the first step toward finding relief.
What Is IBS? Everything You Need to Know About Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal (GI) disorder, meaning it’s not caused by structural damage or disease but by a disruption in how the gut functions.
IBS is characterized by recurrent abdominal pain, discomfort, and changes in your stool and bowel habits.
Cleveland Clinic explains that there are three main subtypes of IBS:
- IBS-C (constipation-predominant): Hard, infrequent stools and straining
- IBS-D (diarrhea-predominant): Frequent, loose stools and urgency
- IBS-M (mixed): A combination of both constipation and diarrhea
Symptoms may also include bloating, cramping, gas, and the sensation of incomplete bowel movements.
Although IBS doesn’t cause long-term damage to the bowel or increase the risk of cancer, it can significantly interfere with daily life.
IBS Causes & Risk Factors
The exact cause of IBS isn’t fully understood, but it’s believed to be influenced by multiple factors.
One key player is the gut–brain axis, the communication network between the central nervous system and the digestive system. When this link is disrupted, it can affect how the gut processes signals, leading to IBS symptoms.
Other common contributing factors include:
- Stress and mental health conditions, such as anxiety or depression
- Genetics, especially if IBS runs in the family
- Gastrointestinal infections (post-infectious IBS)
- Food sensitivities or intolerances, especially to high-FODMAP foods
- Hormonal changes, which may explain why IBS is more common in women
Stress can also worsen symptoms, creating a cycle of discomfort that’s hard to break.
Addressing both the physical and emotional aspects of IBS is often necessary for successful treatment.
How IBS Is Diagnosed
There’s no single test for IBS, which means diagnosis relies heavily on medical history, symptom patterns, and ruling out other conditions.
To rule out other GI conditions like celiac disease, inflammatory bowel disease (IBD), or colorectal cancer, your provider may order:
- Blood tests
- Stool tests
- Colonoscopy or sigmoidoscopy in certain cases
Keeping a symptom diary and noting what you eat, how you feel, and when symptoms flare up can be a helpful tool during the diagnostic process.
IBS Diet & Nutrition – Smart Dietary Strategies for IBS Relief
Food plays a major role in how IBS symptoms show up and how they can be managed.
While no single diet works for everyone, several nutritional approaches have been shown to help people with IBS take control of their symptoms and feel better day-to-day.
Let’s explore some nutritional factors that can help ease symptoms.
High-Fibre, Gut-Friendly Eating
Fibre is an essential nutrient for digestive health, but fibre comes in two main types, and it’s crucial to focus on the right one.
- Soluble fibre: dissolves in water and forms a gel-like substance in the gut. This type of fibre can help soften stool and ease both constipation and diarrhea.
- Insoluble fibre: adds bulk to stool but may trigger symptoms in some people with IBS, particularly bloating or gas.
As you can see, foods rich in soluble fibre are the ones you should be eating if you struggle with IBS. Some of the best sources for insoluble fibre include:
- Oats
- Whole grains
- Vegetables and fruits such as bananas and carrots
- Legumes
While including more fibre in your diet is helpful, it’s important to introduce fibre gradually, increasing your intake over time to avoid triggering excess gas or discomfort.
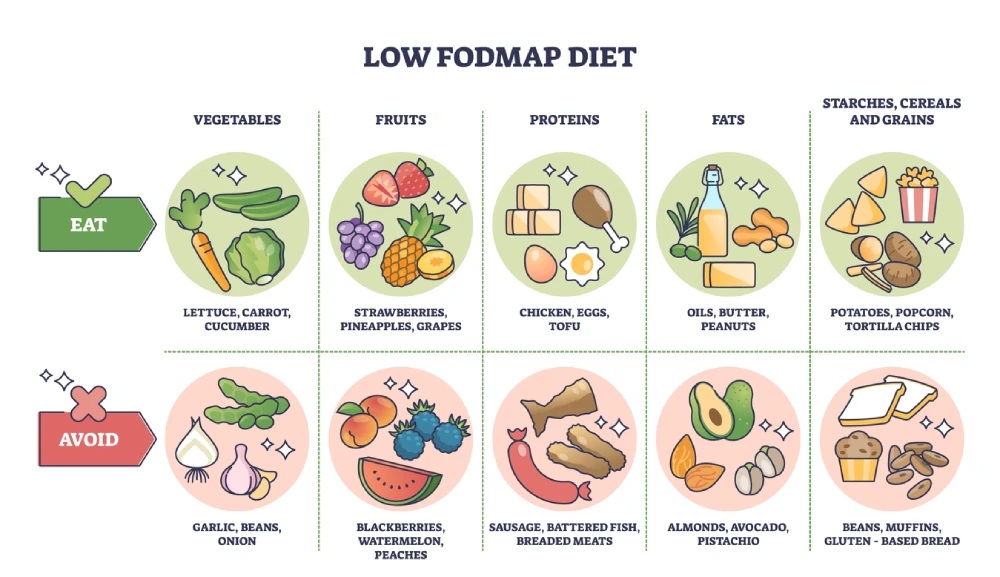
Low-FODMAP Diet
One of the most researched dietary approaches for IBS is the low-FODMAP diet. The Canadian Society of Intestinal Research explains that FODMAPs are carbohydrates that are poorly digested, instead fermenting in the colon, which can aggravate IBS symptoms.
This diet consists of three phases:
- Elimination: removing high-FODMAP foods (e.g., onions, garlic, apples, wheat)
- Reintroduction: slowly reintroducing foods to identify triggers
- Personalization: building a balanced diet based on what you tolerate
A low-FODMAP diet is not meant to be followed long-term without guidance. We strongly recommend working with a registered dietitian to make sure you’re meeting your nutritional needs during and after the process.
Foods to Include & Avoid for IBS
Learning which foods to lean into and which to limit can make a big difference in daily IBS symptom control. Here’s a quick overview:
Foods to include:
- Low-FODMAP fruits and vegetables: carrots, zucchini, bananas, blueberries
- Fermented foods (in moderation): yogurt with active cultures, kefir, kimchi
- Lean proteins and eggs
- Gluten-free grains: quinoa, rice, oats
Foods to avoid:
- High-FODMAP foods: onions, garlic, apples, watermelon
- Dairy (especially milk and soft cheeses)
- Fatty or fried foods
- Caffeinated beverages, including coffee and some teas
- Carbonated drinks, which can contribute to gas and bloating
Making these adjustments doesn’t require perfection, but consistency and mindfulness about how your body reacts are key.
Keeping a food and symptom journal can help identify which foods may be triggering flare-ups for you.
Probiotics, Prebiotics & Fermented Foods
Supporting your gut microbiome is about nourishing your gut with the right kinds of bacteria.
Probiotics, prebiotics, and fermented foods all play unique roles in improving gut health and relieving IBS symptoms when used properly.
What Are Probiotics & Prebiotics?
Probiotics are healthy bacteria that can help restore and maintain a healthy gut microbiome. Think of them as reinforcements for your digestive system, especially when it’s under stress or imbalance.
Prebiotics, on the other hand, are types of fibre that feed the good bacteria already in your gut, helping them grow and thrive.
Together, probiotics and prebiotics form a symbiotic relationship that can support:
- Improved digestion
- Better absorption of nutrients
- Reduced inflammation in the gut
- Enhanced regulation of the gut–brain axis
It’s important to note that results can vary from person to person, and the benefit often depends on the strain, dosage, and duration of use.
Probiotics may take 4 to 6 weeks to show effects, so patience and consistency are key.
Best Food & Drink Sources
While supplements are available, many beneficial microbes can also be found in fermented foods, which are a natural source of probiotics.
Some of the best dietary sources include:
- Yogurt with live and active cultures
- Kefir, a fermented dairy drink rich in multiple strains
- Sauerkraut and kimchi, made from fermented vegetables
- Kombucha, a fermented tea beverage
Try incorporating a small amount of these foods into your routine and observe how your body responds. Not everyone tolerates fermented foods well, so go slow and choose what feels right for your gut.
Lifestyle Strategies to Treat IBS Naturally
Every day habits like hydration, stress management, physical activity, and sleep patterns all play a critical role in keeping your gut functioning smoothly.
Let’s look at how small changes can make a big difference in your IBS symptoms.
Hydration & Eating Habits
Staying well-hydrated is essential for digestive health, especially for people with IBS-C. Water helps keep stool soft and easier to pass, reducing straining and discomfort. Aim for 6 to 8 cups of water per day, and increase your intake if you’re adding more fibre to your diet.
Eating habits also matter. Try to:
- Eat smaller meals more frequently, rather than large, heavy meals
- Chew your food slowly and thoroughly to ease digestion
- Avoid skipping meals, which can lead to irregular bowel movements and bloating
These simple adjustments can help prevent overeating, reduce gas buildup, and keep your digestive system in rhythm.
Stress Management & Gut–Brain Connection
The gut–brain axis is a powerful two-way communication system between your digestive tract and your central nervous system. When you’re stressed, your gut feels it, often triggering IBS symptoms like cramping or urgency.
Mind–body therapies can help calm this connection, such as:
- Mindfulness-Based Stress Reduction (MBSR)
- Cognitive behavioural therapy (CBT)
- Deep breathing, meditation, or guided relaxation techniques
Building even a short daily relaxation practice can improve not only mental well-being but also gut health.
Physical Activity & Gut Health
Regular physical activity can reduce constipation, gas, and bloating, while also improving energy and mood.
Gentle, low-impact activities are often best tolerated, such as:
- Walking
- Swimming
- Yoga, especially poses that encourage abdominal movement
- Cycling or light jogging, depending on tolerance
Aim for 30 minutes of moderate activity on most days of the week. If you’re just getting started, even short walks after meals can help stimulate digestion and reduce post-meal bloating.
Sleep & Daily Routine
Your gut follows a circadian rhythm, just like the rest of your body. That means poor sleep can throw off digestion and trigger IBS flare-ups. To support gut–brain regulation, aim for:
- 7 to 9 hours of quality sleep per night
- A consistent bedtime and wake-up time, even on weekends
- Reducing screen time and caffeine in the hours before bed
Small steps like dimming the lights after dinner or developing a relaxing bedtime ritual can make a real difference in both your sleep and your digestion.
Over‑the‑Counter & Natural Remedies for IBS
For many people with IBS, finding effective symptom relief can involve a combination of natural products and over-the-counter (OTC) medications. These can help manage common issues like bloating, constipation, and diarrhea without immediately turning to prescription therapy.
Fibre Supplements
If you’re not getting enough fibre from food, a supplement may help, particularly for IBS-C. One of the most effective and well-tolerated options is psyllium, such as Metamucil or Option+ Psyllium Hydrophilic Mucilloid available at PharmaChoice pharmacies, a soluble fibre that can regulate stool consistency without causing excessive gas.
Benefits of psyllium include:
- Softening hard stools
- Promoting regular bowel movements
- Supporting healthy gut bacteria over time
Be sure to start low and go slow, gradually increasing your intake with plenty of water to avoid bloating or cramping.
Peppermint Oil & Herbal Aids
Peppermint oil is one of the most researched natural remedies for IBS and has been shown to help relieve:
- Abdominal pain
- Bloating
- Gas
- Intestinal spasms
It works by relaxing the smooth muscles of the gut.
Other herbal options include:
- Chamomile tea, known for its gentle calming effects
- Fennel, which may help reduce bloating and gas
While natural, these remedies aren’t without potential side effects, so it’s a good idea to check with your PharmaChoice pharmacist before adding them to your treatment regimen.
OTC Medications for IBS Symptoms
There are several non-prescription medications that can help manage specific IBS symptoms, including:
- Anti-diarrheals: Loperamide, which helps reduce urgency and frequency for IBS-D
- Laxatives: Osmotic laxatives or stool softeners can aid IBS-C (but use sparingly and under professional guidance)
- Antacids or gas relief tablets: for bloating and discomfort
Your local PharmaChoice pharmacist can recommend personalized OTC options based on your symptom profile and medication history.
It’s always best to get professional guidance before starting a new product, especially if you’re already taking other medications or have underlying health conditions.

IBS Prescription Therapies & Professional Care
If diet, lifestyle, and OTC options haven’t brought enough relief, it might be time to talk to your healthcare provider about prescription therapies.
These treatments are especially helpful for moderate to severe IBS symptoms and are often tailored to your specific IBS subtype.
Common medications include:
- Antispasmodics such as dicyclomine or pinaverium bromide that work to reduce intestinal muscle spasms and cramping
- Antibacterial agents such as rifaximin that help reduce the amount of bacteria in the gut to ease bloating, stomach pain and diarrhea.
- Tricyclic antidepressants such as amitriptyline, that is often used in low doses to modulate pain and gut sensitivity
- SSRIs like citalopram or paroxetine, which can help manage gut–brain interaction and stress-related symptoms
- Guanylate Cyclase-C Agonists, such as linaclotide, that help to stimulate fluid secretion in the intestines to ease IBS-C
These medications are prescribed based on symptom severity, patient history, and other health factors. It’s crucial to have ongoing discussions with a healthcare professional when using prescription medications for IBS.
Working with Health Professionals
IBS is a highly individualized condition, and navigating treatment alone can feel overwhelming. That’s where healthcare professionals come in.
Collaborating with a care team that includes your family doctor, a registered dietitian, and your local pharmacist can lead to more effective and sustainable results.
Key benefits of working with professionals include:
- Dietitian-led low-FODMAP guidance, ensuring balanced nutrition and symptom relief
- Regular medication reviews, especially when combining multiple therapies
- Support with managing IBS triggers like stress, mental health, and sleep
Your PharmaChoice pharmacist is an accessible and trusted partner in your care. We’re here to help you understand your treatment plan, monitor for side effects, and find over-the-counter or prescription solutions that support your digestive and overall health.
Find IBS Support At Your Local PharmaChoice
Living with IBS or digestive discomfort doesn’t have to mean living in discomfort or uncertainty.
With the right combination of gut-friendly foods, targeted probiotics, daily healthy habits, and both natural and medical treatment options, you can take meaningful steps toward feeling better.
At PharmaChoice, we’re here to help you navigate the journey. Whether you’re exploring the low-FODMAP diet, looking for the right fibre supplement, or considering a new prescription medication, our pharmacists are here to offer expert advice tailored to your unique needs.
If you’re ready to take control of your gut health, don’t go it alone.
Speak with your local PharmaChoice pharmacist today for personalized advice, gut health support, and trusted solutions to help you feel your best, right in your community.

