Insulin resistance is a growing health concern, yet many people don’t even realize they have it. This condition, which often has no noticeable symptoms, can lead to serious complications, including type 2 diabetes and heart disease.
However, early intervention can make a significant difference. So how do you know if you’re at risk? What signs should you watch out for, and what steps can you take to manage it?
In this article, we explore the seven common signs of insulin resistance, how it’s diagnosed, and what you can do to improve your health through diet and lifestyle changes. Let’s dive in!
What Is Insulin and Insulin Resistance?
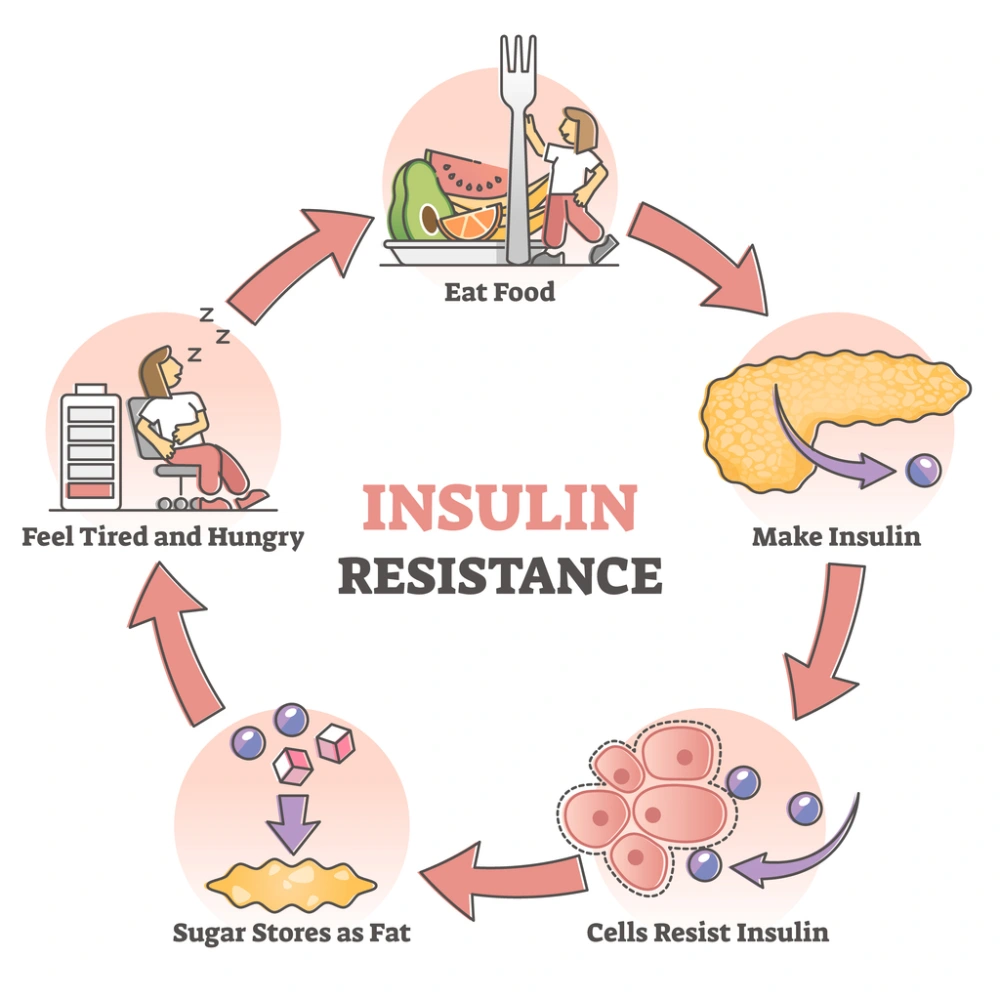
Insulin is a hormone produced by the pancreas that plays a crucial role in regulating blood sugar levels.
When we eat, our body breaks down carbohydrates into glucose (sugar), which enters our bloodstream. Insulin helps glucose move from the bloodstream into our cells, where it’s used for energy.
In a healthy body, this system works efficiently. However, in people with insulin resistance, the body’s cells stop responding properly to insulin, making it difficult for glucose to enter cells.
As a result, the pancreas produces more insulin to help regulate blood sugar levels. Over time, this can lead to high insulin levels (hyperinsulinemia) and, if untreated, can progress to prediabetes or type 2 diabetes.
Insulin resistance is also associated with other conditions, such as metabolic syndrome and cardiovascular disease, making it essential to recognize and manage the condition early.
Risk Factors for Insulin Resistance
While insulin resistance can affect anyone, several risk factors increase the likelihood of developing the condition:
- Obesity: Carrying excess weight, particularly around the abdomen, is a leading risk factor for insulin resistance. Fat tissue, especially visceral fat, releases hormones and inflammatory substances that can interfere with insulin function.
- Sedentary lifestyle: A lack of physical activity reduces the body’s ability to use insulin effectively. Regular exercise can help improve insulin sensitivity by promoting muscle glucose uptake.
- Smoking: Smoking increases inflammation and impairs insulin sensitivity, putting smokers at a higher risk for insulin resistance.
- Sleep issues: Poor sleep quality, especially due to conditions like sleep apnea, has been linked to insulin resistance. Consistent, restful sleep is crucial for maintaining healthy blood sugar levels.
- High cholesterol levels: An imbalance of blood fats, including elevated LDL (bad) cholesterol and low HDL (good) cholesterol, can indicate insulin resistance.
- High blood pressure: Hypertension often occurs alongside insulin resistance, forming part of metabolic syndrome, a cluster of conditions that raises the risk of heart disease and diabetes.
7 Signs & Symptoms of Insulin Resistance
For many individuals, insulin resistance can develop without noticeable symptoms until more serious conditions, such as prediabetes or diabetes, arise.
However, there are subtle signs that may indicate insulin resistance. Being aware of these symptoms allows for early intervention and prevention of more serious complications.
1. Weight Gain
Unexplained weight gain, particularly around the abdomen, can be one of the first signs of insulin resistance.
When insulin levels are high, the body stores more fat, especially in the midsection. This can create a vicious cycle where increased body fat further reduces insulin sensitivity.
Diabetes Canada explains that obesity and other physical signs associated with insulin resistance are more common in children and teens with type 2 diabetes than type 1.
If you’re concerned this may be occurring with your children, speak to your doctor.
2. High Blood Sugar
Even if diabetes hasn’t been diagnosed, high blood sugar levels are a key indicator of insulin resistance.
Blood sugar may rise after meals, especially those high in carbohydrates. Over time, consistently high blood sugar levels can damage organs, nerves, and blood vessels.
3. High Cholesterol
Abnormal cholesterol levels, particularly elevated triglycerides and reduced HDL (good) cholesterol, often accompany insulin resistance.
High cholesterol is a risk factor for heart disease, another condition commonly associated with insulin resistance.
4. Skin Changes (Skin Tags or Patches)
People with insulin resistance may notice skin changes, such as small, fleshy growths called skin tags. Another common sign is dark, velvety patches of skin, particularly around the neck, armpits, or groin.
This condition is known as acanthosis nigricans, and according to Mayo Clinic, most people who have this condition have become resistant to insulin.
5. Fatigue
Insulin resistance can make you feel tired and sluggish.
When the body isn’t efficiently using glucose for energy, it leads to fatigue, even after meals. This can result in feelings of low energy throughout the day.
6. Frequent Urination
As insulin resistance progresses, blood sugar levels can become elevated enough to spill into the urine, causing frequent urination.
This symptom is often associated with diabetes but can appear in the earlier stages of insulin resistance.
7. Tingling in the Feet
Tingling, numbness, or pain in the feet can be an early sign of nerve damage caused by high blood sugar levels.
This symptom, known as diabetic neuropathy, can begin even before diabetes is diagnosed and is often associated with prolonged periods of insulin resistance.
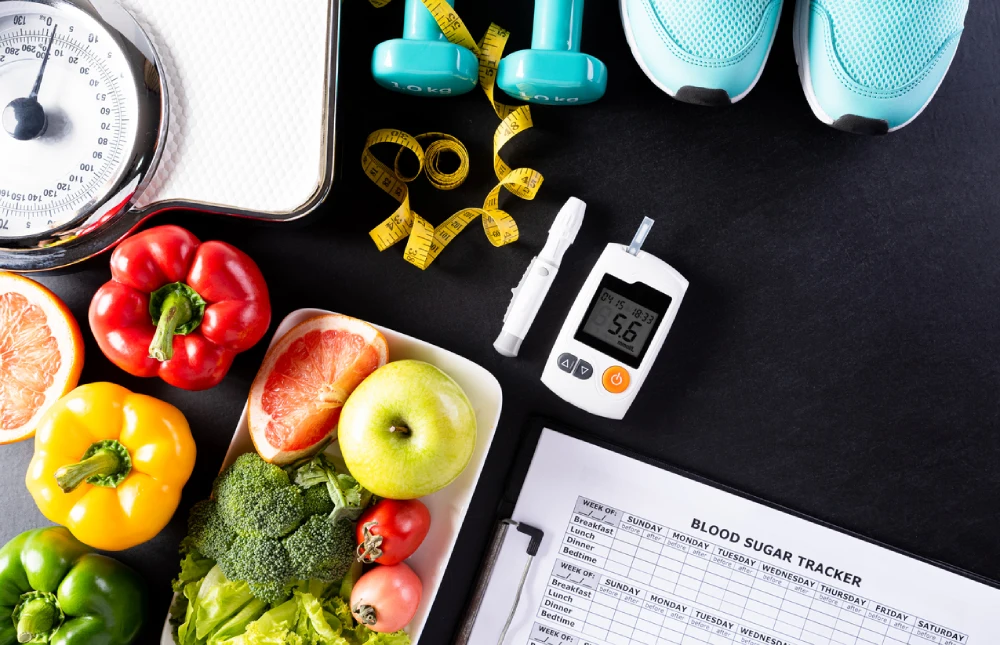
Insulin Resistance Diagnosis + Tests
There is no single test to diagnose insulin resistance, but healthcare providers use a combination of tests and evaluations to determine whether someone is insulin resistant.
Here’s what the process typically involves:
- Health history and physical exam: Your doctor will ask about your family’s medical history, particularly concerning diabetes, and conduct a physical exam to assess your overall health.
- Fasting plasma glucose test: This test measures blood sugar levels after you’ve fasted for at least eight hours. High fasting blood sugar levels may indicate insulin resistance or prediabetes.
- Oral glucose tolerance test: In this test, your blood sugar levels are checked before and after drinking a sugary liquid. The results provide insight into how your body processes glucose.
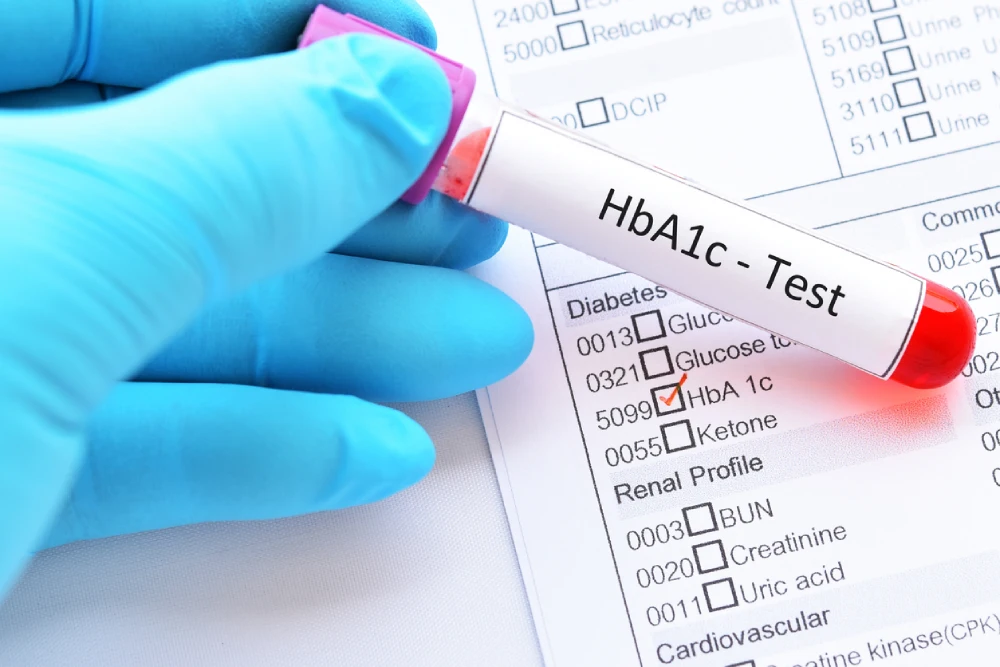
- Hemoglobin A1c test: According to the Annex Naturopathic Clinic, this is one of the most common tests to evaluate blood sugar control. The Hemoglobin A1c test measures your average blood sugar levels over two or three months. An elevated A1c level can indicate prediabetes or diabetes.
- Lipid panel: This blood test measures cholesterol and triglyceride levels. Abnormal results can be a sign of insulin resistance, particularly when triglycerides are high, and HDL cholesterol is low.
How Insulin Resistance Can Progress to Diabetes
Insulin resistance can develop into type 2 diabetes if left untreated.
The progression happens when the pancreas can no longer produce enough insulin to compensate for the body’s resistance. As insulin levels drop, blood sugar levels rise, leading to prediabetes and, eventually, type 2 diabetes.
Diabetes Canada outlines that screening for diabetes should begin at age 40 every three years, or earlier if risk factors, such as obesity or a family history of diabetes, are present.
Prediabetes is diagnosed when blood tests show higher-than-normal blood sugar levels, but not high enough to be classified as diabetes.
Early detection and management can prevent the progression of diabetes, making regular screenings essential for those at risk.
What Causes Insulin Resistance and Prediabetes?
Several factors contribute to insulin resistance and prediabetes, many of which are related to lifestyle and genetics. Understanding these causes can help individuals take preventative measures.
- Extra weight: Excess body fat, particularly around the abdomen, increases the risk of insulin resistance. This is because fat cells, especially in the belly, release hormones that reduce the effectiveness of insulin.
- Lack of physical activity: A sedentary lifestyle decreases the body’s ability to regulate blood sugar. Exercise helps muscles use glucose more effectively, reducing the risk of insulin resistance.
- Health issues: Conditions such as liver problems, polycystic ovary syndrome (PCOS), and gestational diabetes can lead to insulin resistance. Additionally, having a family history of diabetes increases the likelihood of developing the condition.
- Age: Insulin resistance is more common after the age of 45, but younger individuals can also be affected, particularly if they have other risk factors.
- Hormonal imbalances: Hormonal disorders, such as PCOS, can impair insulin function.
- Sleep issues: Sleep apnea and other sleep disorders can disrupt the body’s insulin regulation, increasing the risk of insulin resistance.

Insulin Resistance Prevention – 4 Tips
Preventing insulin resistance is possible, even for those at high risk due to factors like genetics or family history. The following lifestyle changes can help improve insulin sensitivity and reduce the risk of developing more serious conditions:
- Losing weight: Studies have shown that losing just 7% of body weight can reduce the risk of developing diabetes by nearly 60%, according to Mayo Clinic. This can help lower the risk of prediabetes and diabetes.
- Quitting smoking: Smoking not only increases the risk of heart disease but also worsens insulin resistance. Quitting smoking can reduce the likelihood of developing complications related to insulin resistance. Talk to your PharmaChoice pharmacist to learn about quitting smoking aids, and look for the Option+ logo for affordable solutions.
- Regular exercise: Physical activity makes muscles more sensitive to insulin. Aerobic exercises, like walking, running, or swimming, and resistance training can all help improve insulin sensitivity.
- Healthy eating: A diet rich in whole, unprocessed foods can help prevent insulin resistance. Focusing on fibre-rich foods and limiting processed carbohydrates can promote healthy blood sugar levels.
Insulin Resistance Complications (If Left Untreated)
If insulin resistance is left untreated, it can lead to several serious health conditions, including:
- Liver disease: Nonalcoholic fatty liver disease (NAFLD) is closely linked to insulin resistance and can progress to liver inflammation or cirrhosis.
- Eye issues: High blood sugar levels can damage blood vessels in the eyes, leading to diabetic retinopathy, which can cause vision loss.
- Heart disease: Insulin resistance is associated with higher levels of cholesterol and triglycerides, increasing the risk of heart disease and stroke.
- Alzheimer’s disease: Some research suggests a link between insulin resistance and cognitive decline, including an increased risk of Alzheimer’s disease.
Insulin Resistance Treatment
While there is no cure for insulin resistance, managing the condition is possible through lifestyle changes and, in some cases, medications. Doctors may prescribe medications like metformin for those at high risk of developing diabetes.
- Lifestyle changes: Regular exercise, a healthy diet, and losing 5-7% of body weight can significantly improve insulin sensitivity.
- Dietary modifications: Reducing processed foods, eating more fibre, and managing portion sizes can help regulate blood sugar levels. Incorporating healthy fats, lean proteins, and low-glycemic-index foods is also beneficial.
- Stress management: Chronic stress can worsen insulin resistance. Practicing mindfulness, yoga, or deep breathing exercises can help reduce stress and improve insulin sensitivity.
- Sleep: Getting enough quality sleep is crucial for managing insulin resistance. Aiming for 7-8 hours of restful sleep per night can help regulate blood sugar levels.
To learn more about lifestyle or medication options to combat insulin resistance, talk to your PharmaChoice pharmacist.
Living With Insulin Resistance + Recommended Diets
Living with insulin resistance involves making long-term lifestyle changes to manage blood sugar levels and improve overall health. Dietary modifications are an essential part of managing the condition.
- Supplements: Certain supplements, such as cinnamon, ginseng, and magnesium, may help with blood sugar regulation, but it’s important to consult a healthcare provider before adding supplements to your routine.
- Dietary focus: Limiting high-carbohydrate and processed foods, as well as avoiding fatty meats, full-fat dairy and sweets, is key to managing insulin resistance. Instead, focus on fibre-rich foods, such as fruits, vegetables, and whole grains, which have a lower glycemic index and help maintain stable blood sugar levels.
- DASH and Mediterranean diets: These diets emphasize whole, unprocessed foods and healthy fats like olive oil. Both diets have been shown to improve insulin sensitivity and reduce the risk of diabetes.
Learn More About Combatting Insulin Resistance at Your Local PharmaChoice
Recognizing the signs of insulin resistance early can prevent serious health issues like type 2 diabetes. By making proactive lifestyle changes, such as adopting a healthy diet, exercising regularly, and managing stress, you can significantly reduce your risk.
If you’re concerned about insulin resistance, speak with your healthcare provider for personalized advice and testing.
Talk to your pharmacist at your nearest PharmaChoice pharmacy today to learn more about treatment and advice for managing insulin resistance.