Migraines are more than just headaches; they are debilitating neurological events that can significantly impact quality of life.
According to Migraine Canada™, approximately 5 million Canadians live with migraines, enduring recurring bouts of pain, nausea, and sensory disturbances. For many, these episodes can disrupt work, social interactions, and daily activities.
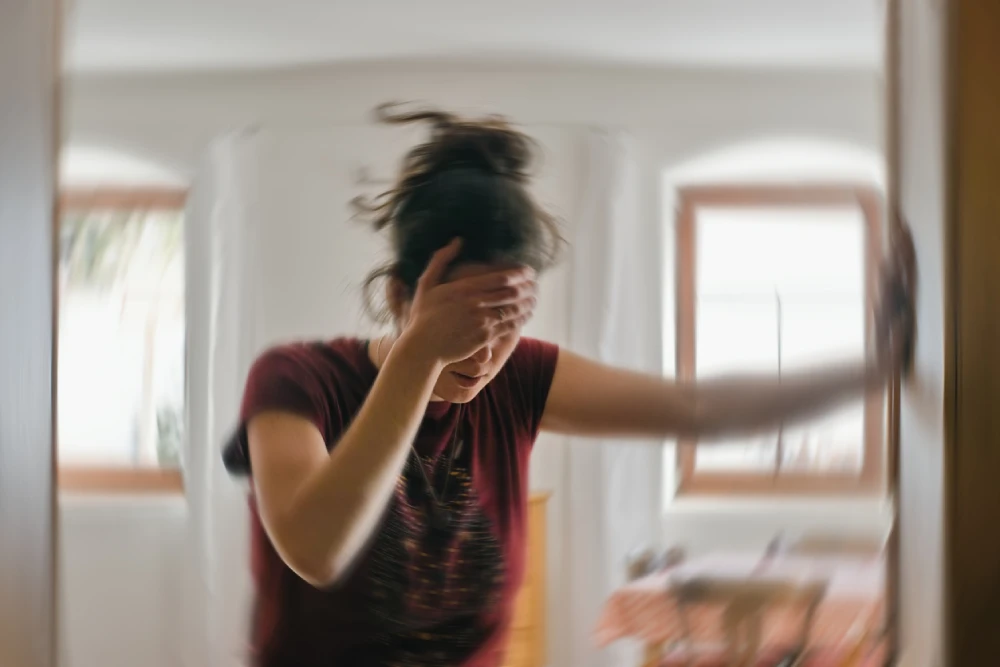
Imagine planning your day only to be sidelined by throbbing pain that makes every sound feel amplified and light unbearable. This is the reality for those dealing with migraines, and finding effective relief can often feel like an ongoing challenge.
Understanding the causes, recognizing the symptoms, and exploring available treatments are essential steps toward finding migraine relief and managing discomfort.
In this comprehensive guide, we’ll dive into the nature of migraines, examine their symptoms and triggers, and explore both conventional and natural treatment options.
Whether you’re living with migraines or supporting someone who is, gaining insight into effective management strategies can make a difference.
What is a Migraine?
Migraines are a type of primary headache disorder characterized by recurrent episodes of moderate to severe headache pain, often accompanied by nausea, sensitivity to light, and sound.
Unlike typical headaches, migraines can last for hours or even days, severely impacting a person’s ability to function in ways they typically would.
One of the biggest challenges with migraines is their unpredictable nature. While some individuals may experience warning signs known as “auras” before the onset of pain, others may find that migraines strike without any notice.
The severity, duration, and accompanying symptoms vary significantly from person to person, making personalized treatment approaches essential.
The Importance of Migraine Awareness
Raising awareness about migraines is crucial because they are frequently misunderstood.
Migraine Awareness Month, observed every June, plays a vital role in educating the public about the impact of this condition and advocating for improved treatment options. During this month, healthcare professionals and organizations come together to share insights, support research, and highlight the real struggles faced by migraine sufferers.
With 50% of people who struggle with migraines being undiagnosed according to the Canadian Migraine Society, awareness becomes more important than ever, empowering patients to seek medical advice rather than dismissing migraines as “just a headache.”
In the following sections, we will explore the types of migraine symptoms, possible causes, diagnostic methods, and the most current treatment strategies.

Types of Migraine and Different Migraine Symptoms
Migraines present differently in each person, but they typically share some common symptoms. Understanding these symptoms can help in early diagnosis and more effective management.
Let’s clear one thing up right from the start: migraines are not just severe headaches; they are complex neurological events that can be completely debilitating and, for some, occur multiple times a month, significantly diminishing the quality of life.
There are two main types of migraine:
- Migraine without aura (also called a ‘common migraine’)
- Migraine with aura (also known as ‘classic migraine’)
Cleveland Clinic shares that there are a few other types of migraine, such as:
- Abdominal migraine (migraines in children)
- Chronic migraine
- Hemiplegic migraine
- Menstrual migraine
- Silent migraine (a migraine without headache)
- Retinal migraine (also called ‘ocular migraine’)
Let’s discuss a couple of the most common types and common symptoms that might occur with each one.
What Are Some Common Migraine Symptoms?
Migraines often present with a variety of symptoms and vary based on the type of migraine. With that said, there are some common symptoms that fall into various categories, such as:
- Throbbing or Pulsating Pain: Often on one side of the head, the pain can range from moderate to severe and may worsen with physical activity.
- Nausea and Vomiting: Many migraine sufferers experience nausea, with some being so intense that they lead to vomiting.
- Sensitivity to Light and Sound: Bright lights and loud noises can intensify the pain, making it difficult to stay in well-lit or noisy environments.
These symptoms can last anywhere from a few hours to several days, depending on the severity and type of migraine.
Managing these symptoms requires a combination of medication, lifestyle adjustments, and sometimes, natural therapies, which we’ll touch on in a later section.
Aura Symptoms
About 25% of people with migraines experience aura, which often happens before the headache phase. The aura length can vary, ranging anywhere between five and 60 minutes long. Some aura symptoms can include:
- Visual Disturbances: These include flashes of light, shimmering spots, or even vision loss in one eye. Some people describe it as looking through cracked glass.
- Sensory Changes: Tingling or numbness in the face or hands may occur, along with difficulty speaking or forming words. You may also experience ringing in your ears.
- Motor Weakness: In rare cases, some individuals may experience temporary muscle weakness.
Aura can be alarming, especially when it first occurs, as it can mimic symptoms of a stroke. However, understanding that these neurological events are temporary and typically subside after about an hour can help in managing anxiety related to aura episodes.
Chronic and Severe Migraines
Some individuals develop more persistent and severe forms of migraines, such as:
- Chronic Migraines: Defined as having migraine symptoms for at least 15 days per month over three months. This condition significantly impairs quality of life and often requires preventive medication.
- Status Migrainosus: As explained by Migraine Canada™, status migrainosis is a debilitating migraine attack lasting more than 72 hours. This form often requires medical intervention.
Managing chronic and severe migraines often involves preventive strategies and specialized care. Early intervention with appropriate treatments can reduce the frequency and severity of these episodes.
Migraine Causes and Triggers
Unfortunately, there is no clear cause of migraines at this time, though it’s known that environmental and genetic factors are key players in their occurrence.
Identifying what triggers migraines can be challenging, as triggers vary from person to person. However, careful consideration and tracking can help you narrow down your unique triggers, helping you better manage your migraines.
Let’s discuss some of the most common causes and triggers of migraines.
Genetic Factors
Migraines often run in families, indicating a genetic component. Studies have shown that individuals with a family history of migraines are more likely to develop them.
This happens because certain gene mutations affecting brain function may predispose a person to migraines. These genetic factors influence how the brain processes pain signals, which can trigger the severe headaches associated with migraines.
Lifestyle and Environmental Triggers
While genetics set the stage, environmental and lifestyle factors often trigger migraine episodes. Common triggers include:
- Stress: Emotional stress can cause tension in muscles and release stress hormones, both of which can trigger migraines.
- Sleep Patterns: Both sleep deprivation and oversleeping can initiate a migraine. Maintaining a consistent sleep schedule is crucial.
- Diet: Foods such as aged cheeses, processed meats, alcohol (especially red wine), and artificial sweeteners may provoke migraines.
- Hormonal Changes: According to Mayo Clinic, women are three times more likely to experience migraines. Hormonal fluctuations, particularly during menstruation, pregnancy, or menopause, play a key role in this.
- Weather Changes: Barometric pressure changes can trigger headaches in some people.
- Noise and Smell: Loud sounds and strong odours, such as perfumes or smoke, may also set off an episode.
- Sensory Overload: Bright lights, flashing screens, or even intense visual patterns can provoke migraines.
- Dehydration: Lack of adequate water intake can increase the likelihood of a migraine.
Identifying Personal Triggers
One of the most effective ways to pinpoint individual triggers is by keeping a migraine diary. Note the following each time a migraine occurs:
- Foods consumed before the episode
- Stress levels and emotional state
- Weather conditions
- Sleep duration and quality
- Physical activity levels
By identifying recurring factors, individuals can work to minimize or avoid specific triggers, leading to a decrease in migraine frequency and severity.

Diagnosing Migraines
Proper diagnosis of migraines requires a comprehensive medical evaluation to rule out other potential causes of headache and to identify the specific type of migraine.
Medical Evaluation
Consulting a healthcare professional is essential for an accurate diagnosis. During a medical visit, the provider will take a detailed history, including:
- Frequency, duration, and intensity of headaches
- Associated symptoms like nausea, visual disturbances, or sensory changes
- Family history of migraines or other neurological disorders
- Physical and neurological examinations help rule out other potential causes, such as infections, brain tumours, or vascular issues.
Diagnostic Tools
If the symptoms are unusual or severe, imaging tests like MRI or CT scans may be ordered to exclude other neurological conditions. Additionally, neurological assessments can help identify abnormalities in brain function or blood flow.
Electroencephalogram (EEG) tests may also be used in cases where seizure-like symptoms are present. These tests can help differentiate between migraines and other neurological disorders.
Acute Migraine Treatment Strategies
Managing migraines effectively requires prompt action at the onset of symptoms. Acute treatment aims to alleviate pain and reduce associated symptoms during a migraine attack.
Choosing the right treatment often depends on the severity of the migraine, individual preferences, and potential side effects of medications.
Over-the-Counter Medications
For mild to moderate migraines, over-the-counter (OTC) medications can be highly effective. These include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications reduce inflammation and alleviate pain, and some common choices include ibuprofen and naproxen.
- Acetaminophen: Works by blocking pain signals to the brain and reducing fever.
- Combination Analgesics: Products containing acetaminophen, ibuprofen, and caffeine can offer more potent relief for some individuals.
PharmaChoice pharmacies offer affordable OTC solutions through their Option+ brand, providing high-quality, cost-effective choices for managing mild migraines.
However, it is essential to use these medications cautiously, as overuse can lead to rebound headaches. Always follow the recommended dosage and consult with a healthcare professional if headaches become more frequent.
Prescription Medications
For moderate to severe migraines that do not respond to OTC treatments, prescription medications may be necessary:
- Triptans: These are specifically designed to treat migraines by stimulating serotonin receptors, which constrict blood vessels and block pain pathways. Common options include Zolmitriptan and Rizatriptan.
- Ergotamines: Such as a Dihydroergotamine injection, which can be effective in treating pain by narrowing blood vessels around the brain.
It is essential to discuss these options with a healthcare professional to choose the most appropriate medication, considering factors such as underlying health conditions and potential side effects.
Non-Pharmacological Interventions
Beyond medications, non-pharmacological strategies can be beneficial, especially when used in conjunction with drug therapy:
- Resting in a Dark, Quiet Room: Reduces sensory overload, allowing symptoms to subside.
- Cold Compresses: Applying a cold pack to the forehead or back of the neck can numb pain and reduce inflammation.
- Hydration: Dehydration can exacerbate migraines, so drinking plenty of water can help alleviate symptoms.
Taking a comprehensive approach that combines medication with lifestyle adjustments often yields the best results in managing acute migraine episodes.
Preventive Measures and Long-Term Management for Migraines
Preventive strategies are essential for individuals who experience frequent or severe migraines. The goal is to reduce the frequency, severity, and duration of attacks, improving overall quality of life.
Preventive Medications
For those who suffer from chronic migraines or have frequent attacks, healthcare providers may recommend preventive medications. These are taken daily, regardless of the presence of symptoms, to reduce the occurrence of migraines.
- Beta-Blockers: These cardiovascular drugs, such as Metoprolol, Nadolol, or Propranolol, help reduce the frequency of migraines by stabilizing blood pressure and calming the vascular system.
- Anticonvulsants (Antiepileptics): Medications like Divalproex, Gabapentin, and Topiramate can decrease migraine frequency by modulating brain activity.
- Antidepressants: Certain tricyclic antidepressants (TCAs) like Amitriptyline or Aventyl (Nortriptyline) can prevent migraines, especially when stress and depression are potential triggers.
- Calcitonin Gene-Related Peptide (CGRP) Inhibitors: Monoclonal antibodies like Aimovig (erenumab), Emgality (galcanezumab), and Ajovy (fremanezumab) specifically target the CGRP pathway, effectively reducing the number of migraine days.
It’s essential to follow the prescribed dosage and monitor for side effects, as these medications can have varying impacts on individuals based on their overall health profile.
Lifestyle Modifications
Adopting healthier habits can make a significant difference in long-term migraine management. Some of these include:
- Regular Sleep: Maintaining consistent sleep patterns helps reduce the risk of sleep-related migraines.
- Balanced Diet: Avoiding known dietary triggers and eating regularly can prevent fluctuations in blood sugar that may provoke migraines.
- Stress Management: Techniques like mindfulness, yoga, and meditation can reduce the physical and emotional tension that triggers headaches.
Consistent lifestyle changes, combined with medical interventions, can significantly decrease the impact of migraines on daily life.
Alternative Therapies
For those seeking complementary approaches to migraine prevention, several natural methods have shown promise:
- Acupuncture: Targeting pressure points can help reduce pain intensity and frequency.
- Biofeedback: Teaches individuals to control physiological functions such as heart rate and muscle tension, potentially minimizing headache severity.
- Cognitive-Behavioural Therapy (CBT): Helps manage stress and emotional triggers through behavioural techniques.
While these therapies may not replace conventional treatments, they can be valuable additions to a comprehensive migraine management plan.
Natural and Complementary Migraine Remedies
Integrating natural therapies can offer additional relief, particularly when combined with conventional treatments. Always consult a healthcare professional before incorporating these methods to avoid potential interactions with current medications.
Herbal Supplements
Some supplements have demonstrated potential benefits in reducing migraine frequency, such as:
- Butterbur: Known for its anti-inflammatory properties, but should be used cautiously as some formulations may contain harmful alkaloids.
- Feverfew: Traditionally used to alleviate headaches, though evidence of efficacy varies.
- Magnesium: Deficiency in magnesium has been linked to migraines, making magnesium a popular choice for supplementation.
Natural remedies should always be discussed with your healthcare team to ensure they do not interact with existing medical conditions, medications or treatments.
Many natural products have interactions with other treatments and should always be reviewed with your pharmacist or primary health care provider before inclusion in your care plan.
Essential Oils and Aromatherapy
Essential oils may offer symptomatic relief:
- Peppermint Oil: Applied to the temples, it can provide a cooling sensation that may help relieve headache pain.
- Lavender Oil: Known for its calming properties, it may reduce stress-induced migraines.
Note: Only use these oils if scents are not a known trigger for your migraines.
Mind-Body Practices
Incorporating relaxation techniques can be beneficial:
- Yoga: Improves circulation and reduces muscle tension.
- Meditation: Helps calm the nervous system, decreasing stress levels.
- Tai Chi: Combines gentle movements with mindfulness, promoting overall well-being.
These practices support the body’s natural ability to manage stress, a common migraine trigger.

Dietary Considerations and Nutritional Support
Diet plays a critical role in managing migraines. Certain foods and dietary habits can either trigger or alleviate migraine symptoms.
Being mindful of what you consume and maintaining a balanced diet can significantly reduce the frequency and intensity of migraines.
Foods to Avoid
Certain foods are commonly associated with triggering migraines. While triggers can vary from person to person, some of the most well-documented dietary culprits include:
- Aged Cheeses: These contain tyramine, a natural compound that can provoke migraines.
- Processed Meats: Items like salami and hot dogs contain nitrates and nitrites, which can dilate blood vessels and trigger headaches.
- Alcohol: Particularly red wine, due to its histamine and sulfite content.
- Artificial Sweeteners: Aspartame, found in diet sodas and sugar-free products, is a known migraine trigger.
- Caffeine: While small amounts can help during an attack, excessive or irregular consumption may trigger migraines.
- Chocolate: Contains both caffeine and beta-phenylethylamine, which can provoke headaches in some individuals.
Keeping a food diary can help identify specific dietary triggers. By recording meals and tracking symptoms, you can better understand which foods may be problematic.
Beneficial Nutrients
Incorporating specific nutrients into your diet can support migraine management:
- Magnesium: Found in leafy greens, nuts, and whole grains, magnesium helps relax blood vessels and may reduce migraine frequency.
- Omega-3 Fatty Acids: Present in fatty fish (like salmon), flaxseed, and walnuts, these acids help reduce inflammation.
- Riboflavin (Vitamin B2): Found in dairy products, eggs, and fortified cereals, riboflavin has been shown to decrease migraine occurrence.
- Coenzyme Q10 (CoQ10): Present in organ meats and whole grains, CoQ10 supports cellular energy production and may reduce migraine frequency.
Incorporating these nutrients into your daily diet can help strengthen your body’s resistance to migraine triggers.
Hydration and Meal Regularity
Staying hydrated is essential for preventing migraines, as dehydration can be a direct trigger. Aim to drink at least eight cups of water daily, especially if you are physically active or live in a hot climate.
Maintaining regular meal times helps keep blood sugar levels stable, which can prevent headaches caused by hypoglycemia. Skipping meals or fasting can increase your risk of a migraine episode.
The Role of PharmaChoice Pharmacists
Managing migraines can be challenging, but the right support can make a difference. PharmaChoice pharmacists are committed to helping you find effective relief through personalized care and expert advice.
Personalized Consultations
Pharmacists understand that every migraine experience is unique. During a consultation, they will:
- Assess your symptoms and discuss your migraine history, current treatment plan, and medications.
- Provide guidance on choosing the right OTC medications.
- Offer advice on lifestyle modifications and trigger management.
By tailoring recommendations to your specific needs, our pharmacists can help you develop a comprehensive plan for migraine management.
Medication Management
With so many treatment options available, managing your medication can feel overwhelming. Our pharmacists can assist by:
- Explaining how to use both acute and preventive medications effectively.
- Providing information on potential drug interactions and side effects.
- Helping you avoid rebound headaches by guiding appropriate usage.
By maintaining an ongoing dialogue with your pharmacist, you can make informed decisions about your treatment plan.
Community Support
PharmaChoice locations are more than just pharmacies; they are community health hubs. Many stores provide access to resources, including information on support groups and educational materials, helping you stay connected and informed.
Visit your local PharmaChoice Pharmacy to learn more about managing migraines and improving your quality of life.
Migraine FAQs
In this section, we’ll address some of the most commonly asked questions about migraines to provide quick, informative answers.
What’s best for migraine relief?
The best migraine relief often involves a combination of approaches, including medications (like triptans or NSAIDs), non-pharmacological strategies (like rest and hydration), and preventive treatments if migraines are frequent.
Personalized care from a pharmacist can help determine the most suitable options for you.
What are the 4 stages of a migraine?
Migraines typically progress through four stages:
- Prodrome: Subtle changes like mood swings or food cravings occur hours or days before the headache.
- Aura: Sensory disturbances, such as visual flashes or tingling, may precede the headache or happen alongside the headache.
- Headache: Throbbing pain, nausea, and sensitivity to light and sound.
- Postdrome: After the headache subsides, individuals may feel drained or fatigued.
Not everyone experiences all four stages, and some may skip the aura phase entirely.
How to sleep with a migraine?
Creating a comfortable sleep environment is key. Use blackout curtains to eliminate light and white noise machines to mask sounds.
Applying a cool compress before bed can also help ease pain. Taking migraine medication prescribed for bedtime can prevent nighttime attacks.
How long can a migraine last?
A migraine attack can last anywhere from 4 to 72 hours. The duration often depends on the type of migraine and how quickly treatment is administered. Chronic migraines may persist longer and occur more frequently, requiring preventive care.
Migraine Management at Your Local PharmaChoice Pharmacy
Managing migraines effectively involves more than just addressing the pain during an episode. Understanding triggers, adopting preventive measures, and choosing the right treatments are essential to living well despite migraines.
Working with healthcare professionals, including PharmaChoice pharmacists, can help develop a comprehensive plan tailored to your needs.
By taking proactive steps—like keeping a migraine diary, making lifestyle changes, and using both pharmaceutical and natural remedies—you can reduce the frequency and severity of migraines.
Whether managing acute attacks or preventing future episodes, consistent care is the key to improvement.
Find migraine relief – Visit your local PharmaChoice pharmacist today for personalized relief options.