Breast cancer is the most commonly diagnosed cancer among Canadian women, with the Government of Canada estimating that 1 in 8 women will face the disease in their lifetime.
That statistic can feel overwhelming, but it highlights why breast cancer awareness is so important. Early recognition of breast cancer signs and symptoms can dramatically improve outcomes.
Imagine noticing a small change in your breast one morning. Would you know if it was serious? Many people hesitate to act, assuming it’s just part of natural changes. But breast cancer can develop quietly, often without pain, and what seems minor could be the first warning sign.
In this guide, we’ll explore the breast cancer signs you should be watching for, risk factors, and diagnosis and treatment options.
How Structure Plays a Role in Breast Cancer
Breasts are made up of glands (lobules), ducts, and a mix of fatty and fibrous connective tissue. Blood vessels, lymph nodes, and nerves are also part of this complex structure.
Understanding the anatomy of the breast is crucial in monitoring your breast health. Where cancer starts often influences how it behaves and what symptoms appear.
For example, the Canadian Cancer Society explains that if the cancer first develops in the duct, a lump in the breast may be the earliest sign, while breast cancer that starts in the lobules (lobular carcinoma) may result in the breast tissue feeling thicker or harder.
Breast density is another important factor to consider. Dense breasts contain more fibrous and glandular tissue than fat. This makes them both a risk factor for cancer and a challenge for mammograms, since dense tissue can mask small tumours.
Knowing your breast density helps you and your healthcare provider choose the right screening tools.
Breast Cancer Explained: How It Develops and Spreads
Cancer starts when changes in a cell’s DNA disrupt normal growth and repair. Instead of following the body’s built-in signals, these cells multiply without control, forming a lump or mass.
As the cancer grows, it can extend into nearby tissue, reach the lymph nodes under the arm, and spread to other parts of the body.
The spread of cancer is not immediate. Often, there is a window of opportunity where the disease is localized and more treatable. This is why acting quickly on symptoms and keeping up with recommended screenings is essential.
Breast Cancer Signs & Symptoms
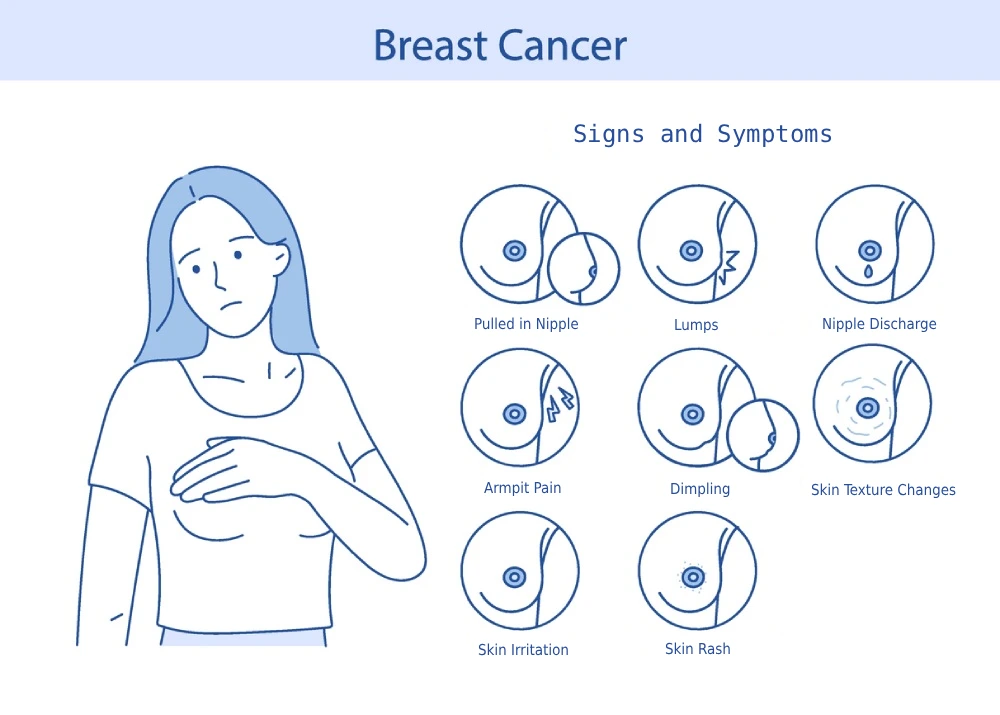
Recognizing the signs and symptoms of breast cancer is one of the most effective ways to catch it early.
Many breast cancers are found by patients themselves during routine self-checks or when they notice something unusual in their daily lives.
While not every change in the breast is cancer, any new, persistent, or unusual symptom should be checked by a healthcare provider without delay.
So, what should you be watching for?
Common Breast Cancer Signs
Breast cancer signs and symptoms can appear gradually or suddenly, and they should always be taken seriously, even if they are not painful. Some hallmark symptoms to watch for, according to the Cleveland Clinic, include:
- A new lump or mass in the breast, often hard and irregular in shape
- Swelling in part or all of a breast, even without a lump
- Breast skin that is dimpled, red, dry, flaky, or thickened
- Changes to the nipple, such as it pointing inward (inverted)
- Nipple discharge that may (or may not) have blood in it
- Underarm lymph node swelling or lump
- A hardened area under the skin
It’s important to note that not every lump is cancerous. However, any new or unusual change should be discussed with your primary care physician.
Less Common But Also Important Breast Cancer Signs
Apart from those warning signs above, there are some less common symptoms that should not be overlooked should they develop. These include:
- Rapid swelling, warmth, redness, and tenderness in the breast. This is often linked to inflammatory breast cancer, and according to Mayo Clinic, can easily be mistaken for a breast infection.
- A red, scaly rash on the nipple and areola. This may be caused by Paget’s disease of the breast and may resemble eczema.
Breast Cancer Symptoms in Men
Although breast cancer is often associated with women, the Quebec Breast Cancer Foundation estimates roughly 270 men are diagnosed in Canada each year.
Key signs include:
- A painless lump under the chest muscle or nipple
- Nipple inversion or skin changes
- Discharge from the nipple
Because awareness is lower in men, diagnosis may be delayed. Any persistent change in breast tissue for men should be checked promptly.
When To Act
If you notice a new change in one or both of your breasts that lasts beyond one menstrual cycle or feels different from your usual pattern, don’t wait. Contact your healthcare provider even if your last mammogram was normal.
How to Tell Normal Changes from Warning Signs
Breasts naturally change with age, menstrual cycles, pregnancy, breastfeeding, medications, and menopause. For example, swelling and tenderness before periods are common, while pregnancy and breastfeeding can make breasts feel nodular.
Several benign (non-cancerous) conditions mimic breast cancer, including:
- Cysts: Fluid-filled sacs, often smooth and movable.
- Fibroadenomas: Solid, non-cancerous lumps found in younger women.
- Mastitis: Inflammation, usually during breastfeeding, that causes pain and redness.
Even though these are benign, you cannot assume a lump is harmless without assessment. Any new or persistent change should still be checked.
A helpful habit is to perform regular self-checks. When performing a self-check, ensure you feel all the tissue of your breast, under your arms, near your lymph nodes, and visually assess for any changes in shape or size in a mirror.
Breast Cancer Risk Factors At a Glance
Understanding risk factors is one of the most powerful steps you can take toward breast cancer awareness.
While having a risk factor does not mean you will develop cancer, it can help guide conversations with your healthcare provider about prevention, lifestyle choices, and screening.
By knowing which risks can and cannot be changed, you’ll be better equipped to protect your health.
Risk Factors Outside of Your Control
Some breast cancer risks are unavoidable. These factors include:
- Age: Risk increases significantly after age 50.
- Sex: Women have the highest risk, though men can also develop breast cancer.
- Family history: A strong pattern of breast or ovarian cancer in close relatives.
- Inherited mutations: BRCA1 and BRCA2 mutations are among the most well-known.
- Personal history: A previous diagnosis of breast cancer or precancerous breast lesions.
- Chest radiation: Particularly treatments received during adolescence.
- Dense breast tissue: Both increase risk and make imaging less sensitive.
Risk Factors You Can Control
Other risk factors are related to lifestyle and reproductive history, meaning there may be opportunities to reduce their impact. Making healthy choices in these areas can lower breast cancer risk.
- Alcohol use: Even low levels of drinking increase risk.
- Obesity: Weight gain, particularly post-menopause, is linked to a higher risk.
- Reproductive timing: Having a first pregnancy later in life, or not having children, can influence risk.
- Menopausal hormone therapy: Long-term use of systemic combined estrogen and progestogen can slightly raise breast cancer risk. This risk varies based on a few different factors, such as duration, regimen and individual factors. Discussing benefits and risks with a healthcare provider helps ensure the safest approach for your individual needs.
What “Higher Risk” Means
Being considered at “higher risk” doesn’t mean cancer is inevitable—it means your healthcare team may recommend more proactive steps.
This can include starting screening at an earlier age, adding MRI or ultrasound to mammography, or discussing genetic testing. Recognizing your level of risk ensures you receive personalized breast health care.
Breast Cancer Types and Subtypes
Not all breast cancers are the same, and understanding the different types is essential for knowing what treatment and prognosis may look like.
Classifying cancer by its origin and biology helps doctors create highly tailored care plans, ensuring patients receive the most effective therapies available.
By Where They Start (Tissue Origin)
Breast cancers are often categorized based on where they begin in the breast structure. These types include:
- Ductal carcinoma in situ (DCIS): A non-invasive cancer limited to the ducts.
- Invasive ductal carcinoma (IDC): One of the most common types, spreading beyond the ducts.
- Lobular carcinoma (ILC): Starts in the lobules and often spreads to nearby tissue.
By Receptor Status and Biology
Each cancer is also tested for receptors that affect how it grows and responds to treatment. Knowing your receptor status is crucial in guiding treatment:
- Hormone receptor positive (ER and/or PR): Grows with estrogen or progesterone.
- HER2 positive or HER2-low: Cancers that have high levels of the HER2 protein or have lower but targetable levels.
- Triple-negative breast cancer (TNBC): Lacks hormone and HER2 receptors, tends to be more aggressive, and requires different treatment strategies.
Your subtype determines which therapies are most effective, making this classification one of the most important factors in breast cancer treatment planning.
Breast Cancer Screening and Early Detection Tools
 Screening is the cornerstone of early detection, helping identify cancer before symptoms develop. When combined with personal awareness of breast changes, it can dramatically increase the chances of successful treatment.
Screening is the cornerstone of early detection, helping identify cancer before symptoms develop. When combined with personal awareness of breast changes, it can dramatically increase the chances of successful treatment.
Knowing the tools available and when they are recommended helps you advocate for the right care.
- Mammography: The most common screening tool, effective for detecting small tumours but less sensitive in dense breasts.
- Ultrasound: Often used when a lump is detected or as a supplement in dense breasts.
- MRI: Recommended for people at higher risk, such as those with BRCA mutations or very dense breast tissue.
Women aged 50–74 are generally offered routine mammograms, but timing and frequency can differ for those with higher risk. Asking questions about your breast density and screening options can help you and your doctor approach your care in an individual way that supports your unique risk factors.
How Breast Cancer Diagnosis Is Confirmed
If a screening test or symptom raises concern, the next step is diagnosis. Diagnosis involves multiple steps, each of which adds detail to the picture of what’s happening inside the breast. The goal is not only to confirm cancer but also to understand its stage, biology, and behaviour.
- Clinical breast exam: A hands-on check by a healthcare provider for any lumps or concerning changes in breast tissue.
- Imaging: Targeted mammograms, ultrasounds, or MRIs provide more detail about suspicious areas.
- Biopsy: Tissue sampling is the gold standard for diagnosis, confirming whether cells are cancerous.
The pathology report from a biopsy will outline tumour type, grade, stage, and receptor/HER2 status. This information drives the treatment plan and gives patients clarity about what lies ahead.
Breast Cancer Treatment – Not One-Size-Fits-All
Breast cancer treatment is highly individualized. Doctors consider the stage, subtype, overall health, and patient preferences before building a care plan. This personalized approach ensures treatments target the cancer effectively while balancing quality of life.
Local Breast Cancer Treatments
These treatments focus directly on the breast and surrounding tissues:
- Lumpectomy: Removing the tumour and a margin of surrounding tissue.
- Mastectomy: Removing one or both breasts, sometimes including reconstruction options.
- Lymph node surgery: Checking for spread and preventing further progression.
- Radiation therapy: Targeting residual cancer cells after surgery.
Systemic Therapies
These treatments circulate throughout the body to target cancer cells wherever they may be:
- Chemotherapy: Attacks rapidly dividing cancer cells.
- Endocrine therapy: Blocks hormones that drive growth in hormone-positive cancers.
- Targeted therapy: Drugs designed to interfere with specific proteins such as HER2.
- Immunotherapy: Harnesses the immune system to recognize and fight cancer.
By combining local and systemic therapies, many people achieve long-term remission and live full, healthy lives.

Living Well During and After Breast Cancer Treatment
Breast cancer awareness is about more than knowing the facts—it’s about paying attention to your own body and taking action when something feels different.
By understanding risk factors, recognizing signs and symptoms, and keeping up with recommended screenings, you give yourself the best chance for early detection and effective treatment.
Today, there are many treatment options available, and countless people go on to live full and healthy lives after a breast cancer diagnosis.
Remember, you are not alone on this journey. Your healthcare team, along with your local PharmaChoice pharmacist, is here to support you with trusted advice, medication guidance, and community resources every step of the way.
If you’ve noticed a change or have questions about breast health, visit your local PharmaChoice pharmacist or family doctor for trusted advice and support tailored to your community.