Living with arthritis means facing more than just joint pain. For millions of Canadians, it can impact daily routines, mobility, mental health, and overall quality of life.
Arthritis is one of Canada’s most common chronic diseases, yet it is often misunderstood or dismissed as a condition that only affects older adults.
The truth is that arthritis can affect anyone, including children and young adults, and early recognition is key to managing symptoms effectively.
In this guide, we will explore arthritis symptoms, types, and treatment options while sharing practical management tips for those living with arthritis.
Our goal is to help you better understand arthritis, recognize when to seek help, and feel confident about the treatment and support available, including from your local PharmaChoice pharmacist.
Arthritis 101: What It Is and Why Awareness Matters in Canada
Arthritis is not simply “aches and pains.” It is a chronic, often progressive condition that involves inflammation, damage, or degeneration in the joints.
According to Arthritis Research Canada, arthritis affects more than 6 million people across the country, making it Canada’s most common chronic disease.
Considered an invisible illness, many people with arthritis do not “look” sick, despite the toll their condition can have on their quality of life. This can make it harder for others to understand the daily challenges they face.
So, let’s shine a light on some important statistics. According to Arthritis Society Canada, people with arthritis are:
- Twice as likely to be out of the workforce
- Experience pain that limits daily activities
- Twice as likely to struggle with their mental health
- Five times more likely to face mobility challenges
Furthermore, half of the people with arthritis are below the age of 65, with women and those assigned female at birth being at a higher risk than their male counterparts.
While there is no cure, many treatments can manage symptoms and slow disease progression, especially when arthritis is diagnosed early.
Raising awareness helps break down misconceptions, encourages early diagnosis, and ensures people get the support they need.
Arthritis Types: Breaking Down the Main Categories
Arthritis is a complex condition, with more than 100 different types. However, despite the many variations, they are generally grouped into a few key categories.
1. Degenerative Arthritis
Typically referred to as Osteoarthritis (OA), degenerative arthritis is the most common type people develop.
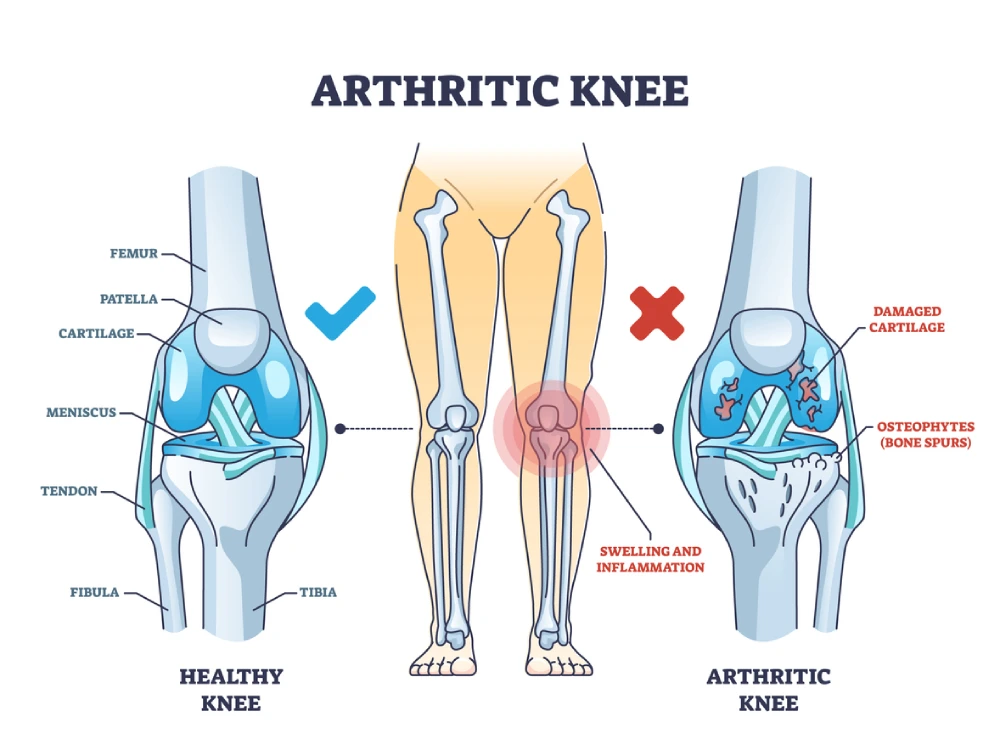
This type of arthritis occurs when the cartilage in joints wears down over time, often affecting weight-bearing joints such as the knees, hips, and spine.
This “wear and tear” leads to pain, stiffness, and reduced mobility in the affected joints.
2. Inflammatory Autoimmune Arthritis
These forms occur when the immune system mistakenly attacks healthy joint tissue, causing inflammation and damage. Some of the most common types include:
- Rheumatoid arthritis: Often affects multiple joints symmetrically, such as both wrists or knees
- Psoriatic arthritis: Affects some people with psoriasis, causing joint pain, swelling, and skin symptoms
- Ankylosing spondylitis (axial spondyloarthritis): Primarily affects the spine, and can result in some of the vertebrae of the spine fusing. This causes stiffness and reduced flexibility.
3. Crystal-Induced Arthritis – Gout
Gout and pseudogout are the most common types that fall into this category and occur when crystal deposits develop in the joints, typically due to an increase in uric acid in the blood.
This can cause sudden, severe pain and swelling in the affected joint.
4. Juvenile Arthritis
The types of arthritis that fall into this category are those that affect children under the age of 16.
Symptoms may include persistent joint swelling, stiffness, pain, and difficulty with daily activities like walking or writing and may even affect growth and development.
Understanding your arthritis type is crucial because treatment strategies vary significantly between osteoarthritis and inflammatory types.
Risk Factors and Arthritis Symptoms
While aging increases the likelihood of developing arthritis, several additional factors play an important role in risk.
Key risk factors include:
- Family history: If arthritis runs in your family, your risk may be higher due to genetic predisposition.
- Excess weight: This adds extra strain to joints, particularly the knees, hips, and spine, and can speed up joint wear.
- Previous joint injury: Sports injuries, fractures, or repetitive strain can increase vulnerability later in life.
- Gender: 1 in 4 women are diagnosed with arthritis compared to 1 in 6 men.
Common arthritis symptoms to watch for:
- Persistent joint pain or tenderness
- Stiffness, especially in the morning or after rest
- Swelling, redness, or warmth around joints
- Reduced range of motion or flexibility
- Fatigue or feeling unwell alongside joint symptoms
If you notice these signs for more than two weeks, consult your healthcare provider for assessment. Early detection allows for more effective treatment and improved quality of life.
How Is Arthritis Diagnosed?
Diagnosing arthritis involves more than simply identifying joint pain. Your healthcare provider will combine several approaches to confirm the type and severity you’re experiencing.
1. Clinical history and physical examination
Your doctor will discuss your symptoms, medical history, and any family history of arthritis. They will also assess your joints for tenderness, swelling, redness, and movement limitations.
2. Laboratory tests
These can help pinpoint the type of arthritis, and may include tests that look for:
- Inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), a test that measures the speed at which red blood cells fall to the bottom of a blood vial over a set amount of time
- Autoantibodies such as rheumatoid factor (RF) and anti-CCP for rheumatoid arthritis
- Uric acid levels to diagnose gout
3. Imaging studies
There are a few common imaging tests that may be ordered to help your doctor get a better sense of what may be causing your symptoms, such as:
- X-rays: can show bone changes and joint space narrowing
- Ultrasound and MRI: used to detect inflammation and early damage before it appears on X-ray
A clear diagnosis allows your healthcare team to tailor your treatment for the best results.
Arthritis Treatment Options & Outcome Goals
The right treatment approach depends on whether arthritis is degenerative (like osteoarthritis) or autoimmune/inflammatory (like rheumatoid arthritis). Both require careful management, but the strategies differ.
Let’s explore some of the treatment options for each.
Osteoarthritis Treatment Options
An effective approach for osteoarthritis treatment often combines lifestyle changes, medications, and supportive therapies tailored to your needs.
Lifestyle and physical therapy
Staying active is one of the most powerful tools in managing osteoarthritis. Regular low-impact exercise, such as swimming, cycling, or walking, helps to strengthen the muscles around joints and improve stability.
Physiotherapists can design individualized programs to maintain range of motion, reduce stiffness, and lower the risk of further injury.
Medications
- Acetaminophen and NSAIDs like Option+ ibuprofen and naproxen can help with pain and inflammation
- Topical NSAIDs like diclofenac gel (Voltaren) may be used for arthritis that affects the knees
Other interventions
- Joint injections (such as corticosteroids or hyaluronic acid) may be offered when oral or topical treatments are not enough
- Surgical options like joint replacement are considered for severe damage
Inflammatory Arthritis Treatment Options
Inflammatory arthritis requires treatment to reduce immune system activity and protect joints from damage.
This is typically done through the use of specific medications.
Some of the main medication classes include:
- Conventional Synthetic Disease-Modifying Antirheumatic Drugs (DMARDs) such as hydroxychloroquine and sulfasalazine, which work to combat inflammation or medications that suppress the immune system, such as methotrexate and leflunomide
- Biologics such as adalimumab, etanercept, and rituximab, which block specific parts of the immune system that drive inflammation
- Janus kinase inhibitors, such as upadacitinib, for patients who do not respond to other treatments
- NSAIDs and corticosteroids to control pain and inflammation during flares
Treat-to-target approach
Inflammatory arthritis care often follows a treat-to-target strategy. Your healthcare team will track disease activity through regular assessments and adjust medications until you reach remission or low disease activity.
This approach reduces the risk of long-term damage and helps preserve mobility and quality of life.
Pharmacist support
Pharmacists are a key member of your care team. They can help guide you in choosing appropriate over-the-counter products, explain prescription medications, and recommend home aids like braces, walking supports, or heat and cold therapy products.
Talk to your Pharmachoice pharmacist today about the affordable Option+ products that may help support your arthritis treatment plan.
Arthritis Treatment Goals
Because there is no cure for arthritis, treatment aims to manage the condition, provide relief where possible and improve function and quality of life.
Some of the most common treatment goals include:
- Control pain and inflammation so you can maintain daily function
- Preserve mobility to keep joints as flexible as possible
- Slow disease progression in inflammatory types to prevent damage
- Prevent treatment side effects by using the safest, most effective options
Arthritis treatment plans are individualized, balancing lifestyle changes, medications, and other therapies to meet each patient’s unique needs.

Self-Management Tips for Arthritis
Living well with arthritis is not only about following medical treatments—it also involves consistent daily habits that protect your joints and support overall well-being.
By combining physical activity, healthy lifestyle choices, and the right support tools, you can help reduce discomfort and maintain independence.
Here are a few strategies you can use to support your treatment regimen:
- Stay active with low-impact exercises like swimming, cycling, or tai chi to maintain flexibility and strength
- Maintain a healthy weight to reduce strain on joints and slow wear and tear
- Support your mental health through counselling, support groups, or mindfulness practices
- Prioritize rest and sleep to allow your body to recover and manage inflammation
- Use assistive devices such as canes, braces, or ergonomic tools to make daily activities easier
Arthritis Myths, Mistakes, and Misinformation
When it comes to arthritis, misinformation can cause people to delay seeking help or choose treatments that are not effective. Separating fact from fiction is essential for managing the condition successfully.
Let’s break some of the most common myths about arthritis.
- “Arthritis only happens when you get older.” – Arthritis can develop at any age, from childhood to later years. Certain types, like juvenile arthritis, specifically affect children and teens.
- “Rest is always better than movement.” – While rest can help during acute flares, prolonged inactivity often leads to muscle weakness and reduced joint function. Safe, guided movement is usually part of a healthy management plan.
- “Topicals do not work.” – Evidence shows that topical NSAIDs, such as diclofenac gel, can significantly reduce pain in arthritis that affects the knee.
- “NSAIDs are safe for daily use without guidance.” – Long-term use can increase the risk of gastrointestinal, kidney, and heart issues. These medications should always be taken under medical or pharmacist supervision to ensure safety.
Knowing the truth about arthritis empowers you to take the right actions early and avoid mistakes that could worsen symptoms or delay proper treatment.
When to See Whom: A Simple Care Pathway
Arthritis care often involves a team of healthcare professionals. Understanding when and where to seek help ensures you get the right care at the right time, preventing delays that could lead to joint damage.
- Family doctor: For ongoing symptoms or suspected arthritis, and to coordinate referrals
- Rheumatologist: For inflammatory arthritis or when standard treatments are not working
- Pharmacist: For OTC medication guidance, side effect checks, and product recommendations for pain relief and mobility support
- Urgent care or emergency: If you experience sudden, severe joint pain, swelling, fever, or inability to move a joint
Find Arthritis Support at Your Local PharmaChoice Pharmacy
Early diagnosis and the right treatment plan can slow arthritis progression, reduce symptoms, and help you maintain independence.
Your local PharmaChoice pharmacist can help you manage medications, recommend products, and support your care plan. We can also connect you with other healthcare providers when needed.
Visit your local PharmaChoice pharmacy today for personalized arthritis support, expert medication guidance, and trusted care right in your community.



